How confident are primary care clinicians in diagnosis and management of respiratory conditions? (ID 568)
University of Oxford
Abstract
Aim:
In the UK, diagnosis and management of common respiratory conditions is mainly delivered by primary care, but diagnostic testing, including spirometry and fractional exhaled nitric oxide (FeNO) is not widely available. NHS funding is being directed towards increased community provision of diagnostic testing and breathlessness pathways. We aimed to assess confidence levels amongst primary care clinicians in diagnosing and managing common respiratory presentations, as a needs evaluation to inform service development.
Method:
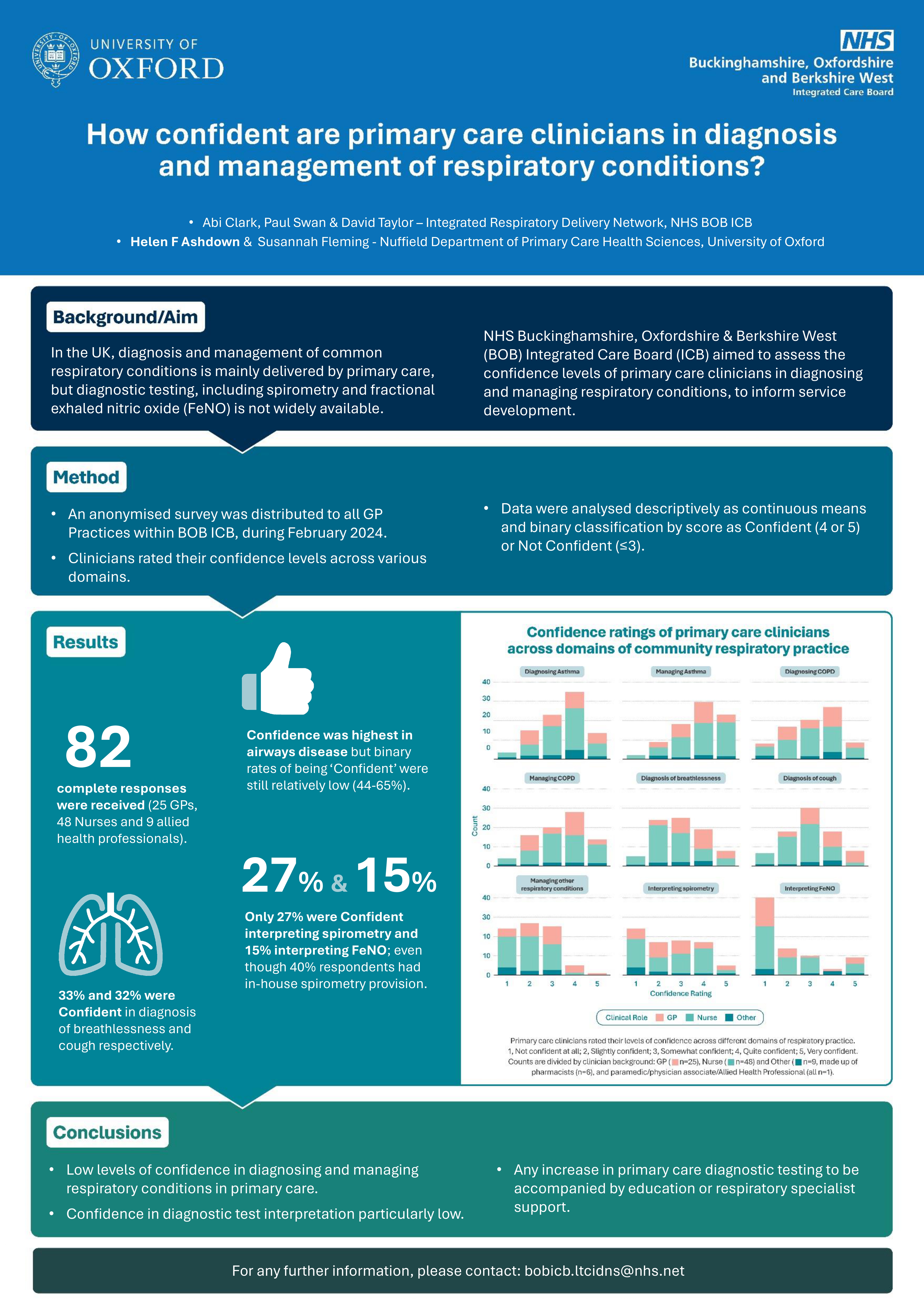
An anonymised survey was developed by the Integrated Respiratory Delivery Network of the Buckinghamshire, Oxfordshire and Berkshire West (BOB) Integrated Care Board (ICB). After piloting and revision, the survey was distributed in February 2024 to all BOB ICB GP practices, and via a regional e-mail network of respiratory-interested clinicians. Clinicians rated their levels of confidence across various domains. Data were analysed descriptively as continuous means and binary classification by score as Confident (4 or 5) or Not Confident (≤3).
Results:
We received 82 complete responses (25 GPs, 48 nurses and 9 allied health professionals (Figure)). Confidence was highest in airways disease but binary rates of being ‘Confident’ were still relatively low (44-65%). 33% and 32% were Confident in diagnosis of breathlessness and cough respectively. Only 27% were Confident interpreting spirometry and 15% interpreting FeNO, even though 40% respondents had in-house spirometry provision.
For most domains there was no significant difference between confidence scores between GP and nurse subgroups, but GPs were significantly more confident at diagnosing breathlessness and cough (both p<0.001) and managing non-asthma/COPD respiratory conditions (p=0.01).
Conclusion:
Our results highlight low levels of confidence amongst primary care clinicians, particularly in diagnostic test interpretation. While there are benefits to holistic care in a community setting, our findings identify a need for any increase in primary care diagnostic testing to be accompanied by education or respiratory specialist support.
Funding: This work was funded by Buckinghamshire, Oxfordshire and Berkshire West (BOB) Integrated Care Board (ICB).
HFA receives funding from the NIHR HealthTech Research Centre in Community Healthcare at Oxford Health NHS Foundation Trust. The views expressed are those of the author(s) and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care.
Conflicts of interest: AC, PS, and DT work within the BOB ICB: AC as Project Manager for Long-Term Conditions; PS as Strategy Development Lead and Respiratory Clinical Network Manager; DT as Secondary care lead and co-Chair of the IRDN.